What is intestinal Failure and what happens after intestine failure?
Intestinal failure is defined as reduction in functioning length of small intestine below a certain limit, which causes inability to digest and absorb nutrients and fluid, required for adequate maintenance of an individual. Most cases of intestinal failure are due to ‘Short Gut Syndrome’ which is due to surgical resection leading to loss of functioning mass of small intestine.
The small intestine is a muscular tract that follows the stomach. This is the place where most of digestion and absorption of food, fluids, electrolytes and nutrients takes place. Any problem in proper functioning of the small intestine can make a person dehydrated and malnourished. Intestinal failure can also cause diarrhoea, muscle wasting, poor growth, frequent infections, weight loss and fatigue.
How does a person survive after the removal of small intestine?
In case of failure of small intestine the usual process of eating and digestion cannot take place and hence parenteral nutrition (PN) is used to feed the patient. The feeding is done intravenously- infusion of fluids directly into aan intravenous catheter placed into one of the large veins of the body. . Depending on the need of the person, which can vary individually, PN formula is made and nutrients such as glucose, amino acids, lipids, vitamins and minerals are given to the patient. The process is called total parenteral nutrition (TPN) when no significant nutrition is obtained by other routes.
Is TPN a permanent solution?
A patient with intestine failure can nutritional requirements through TPN. It is observed that patients can live on TPN for many years. However, dependency on this process of feeding has a major impact on the patient’s quality of life, Complications of TPN can further impair normal life, such as infections of the venous line which can be life threatening; the liver becomes fatty when on long term TPN and can get scarred which eventually leads to end stage liver failure.. Patients in whom more than 75% of functional intestinal length is removed surgically or has < 50 cm of small intestine may have permanent dependence on TPN and thus higher incidence of associated complications. Intestinal transplantation should be offered to such individuals before significant complications arise.
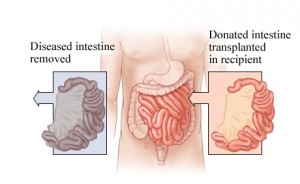
How is intestinal transplant done?
A transplant requires surgical removal of small intestine and its replacement with a healthy organ. There are three main types of intestinal transplantation :
- Isolated small intestine
- Combined liver & intestine
- Multivisceral, which contains small intestine with stomach, duodenum, pancreas, with/without liver
There are two ways by which an intestinal graft can be obtained, either from a brain dead donor or from a living related donor. In case of brain dead donor, whole length of the small intestine can be utilised for transplantation whereas in case of living donor approximately 40% of the small intestine(normal length of small intestine is between 600-800cm) can be removed without any major complications to the living donor.
. Initially the blood vessels of the patient and donor are connected to establish blood supply to the transplanted intestine. Gradually the donor’s intestine is connected to the patient’s gastrointestinal tract. Ileostomy is performed after this. The process involves surgically created opening through which the ileum (a part of the small intestine) is brought out through the abdominal wall. This opening allows regular monitoring via biopsies to check for rejection. The aim is to commence enteral feeding as early as possible after transplantation. Majority of the patients are able to have ileostomy closed and normal intestinal continuity restored over a period of time.
Why intestine transplant so complicated?
Before 2001 intestinal transplant was largely considered experimental. In the past decade it is evolving as a standard care for patients with intestinal failure. When compared to liver and kidney the intestine is a difficult organ to transplant. The gut has a large number of lymphoid tissue and bacteria which can cause rejection or infection after the transplant. Patients are given heavy dose of anti rejection drugs which suppresses their immune system so that the body will accept the transplanted intestine.
The suppression of immune system puts them at higher risk of infection as compared to other patients. Also there may be rejection, intestinal ischemia (injury from inadequate blood supply) and fluid leaks. Although all this can be treated but in some cases it may cause graft loss or even the patient’s death. There are very few attempts to perform Intestinal transplant in India, hence no definite success rate is known, however 1 year and 3 year survival is reported to be close to 80 % and 67% in the Western countries. Patients with irreversible intestinal failure who were initially viewed with nihilistic attitude now have an option of leading a near normal life with Intestinal transplantation.
Dr Naimish Mehta is the Lead HPB and Liver Transplant Surgeon, in the Deptt of Surgical Gastroenterology & Liver Transplant Unit I, Sir Ganga Ram Hospital, New Delhi. Dr Naimish Mehta has performed several successful Intestinal Transplant Surgery in Delhi, India as considered to be one of the best Intestinal Transplant Surgeon in Delhi, India